The coronavirus disease (COVID-19) is spreading, and with it many doubts, concerns and information that is inaccurate or unsubstantiated. To provide you with the latest and most credible information regarding breastfeeding, human milk, safety and health for you and your baby, Medela has created this COVID-19 information hub concerning breastfeeding with a collection of questions and answers to help you cope with this new reality we are now living. We will update this Q&A frequently as new information becomes available.
Share this information with your family, friends and colleagues. Help other parents to get answers from reliable and trustworthy sources.
—
Pregnancy
I am pregnant. Will it hurt the baby if I have COVID-19 during the pregnancy?
According to the CDC, at this time, there is not enough evidence to determine whether the virus is transmitted from a mother to her baby during pregnancy, or the potential impact this may have on the baby. This is currently being investigated.at this time. A small number of problems with pregnancy or delivery (e.g. preterm birth) have been reported in babies born to mothers who tested positive for COVID-19 during their pregnancy. However, it is not clear if these outcomes were actually related to maternal infection or not.
—
I am pregnant. Is it easier for pregnant women to become ill with COVID-19?
The Royal College of Obstetricians and Gynaecologists state that pregnant women do not appear to be more susceptible to the consequences of infection with COVID-19 than the general population. Pregnant women experience changes in their bodies that may increase their risk of some infections. It is known that with viruses from the same family as COVID-19, and other viral respiratory infections, such as influenza, women have had a higher risk of developing severe illness. This is why the CDC says it is always important for pregnant women to protect themselves from illnesses.
—
I am pregnant. How do I protect myself from COVID-19 during the pregnancy?
Pregnant women should do the same things as the general public to avoid infection. Please see the answer to the question How can I protect myself and others?
—
What if I am pregnant and meet with somebody who has the virus, will I be able to breastfeed?
Yes. Breast milk is the best nutrition for most infants. Breast milk provides protection against many illnesses. According to the Academy of Breastfeeding Medicine, WHO and the CDC, if you intend to breastfeed or provide milk to your baby, even if you have been exposed to the coronavirus or have symptoms, you are encouraged to breastfeed. If you could be infectious, you must however apply all the necessary precautions to avoid spreading the virus to your infant, including washing your hands before holding your baby, and wearing a face mask when in close contact with your baby as, for example, during direct breastfeeding.
—
What happens when a woman with COVID-19 gives birth?
According to AAP new guidance on July 22, 2020 regarding separation of mums and babies, it is possible for mothers with suspected or confirmed COVID-19 to room-in with their newborns when precautions are taken to protect the infants from maternal infectious respiratory secretions.
According to the CDC, if there is need for prolonged temporary separation is prolonged, primarily because the mother needs medical care for herself, providing the baby with expressed breast milk is recommended. If possible, a dedicated breast pump should be provided. If it is not possible to dedicate a breast pump to a COVID-19 positive mother, the mother can use a multi user breast pump. Special care must be taken to clean and disinfect the breast pump prior to it being used by another mother. Please see the answer to the question What is the recommendation for use of Medela equipment if a mother is hospitalised due to Coronavirus disease? in the section for Using breast pumps and other products questions.
Johns Hopkins Medicine states that once the mother’s symptoms improve and she and her baby are ready to be discharged home, it is possible for her to either continue using expressed breast milk or to breastfeed, taking the necessary precautions to avoid spreading the virus to her infant. These include washing hands before holding her baby, and wearing a face mask when in close contact with her baby.
—
Breastfeeding
Can I breastfeed if I am diagnosed with COVID-19?
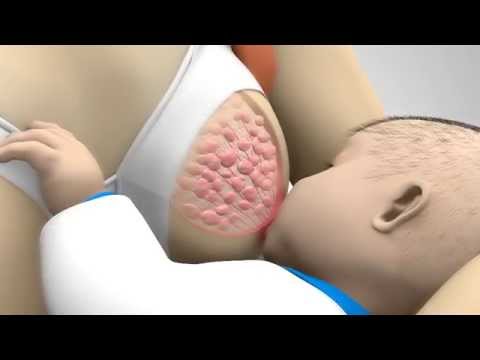
UNICEF, the Academy of Breastfeeding Medicine, WHO and the CDC state that considering the benefits of breastfeeding and the insignificant role of breast milk in the transmission of other respiratory viruses, the mother can continue breastfeeding, while applying all the necessary precautions. There is limited evidence for the presence of viral RNA in breast milk, while there is neither evidence for active virus in breast milk nor transmission via breast milk. Currently, the primary concern is not whether the virus can be transmitted through breast milk, but rather whether an infected mother can transmit the virus through respiratory droplets during the period of breastfeeding. Precautions to avoid spreading the virus to your infant include washing hands before holding your baby, and wearing a face mask when in close contact with your baby as, for example, during direct breastfeeding. Consult with your health care provider if you have questions or concerns.
Recent research has shown specific benefits of providing breast milk relevant to the COVID-19 situation. Researchers in China and in USA have recently found antibodies against the new coronavirus in the milk of mothers who had previously had COVID-19, further supporting the recommendation to continue breastfeeding.
—
Can COVID-19 be transmitted through breast milk?
UNICEF, the Academy of Breastfeeding Medicine, WHO and the CDC report that the limited studies on breastfeeding women with COVID-19 and other coronavirus infections have not detected the virus in breast milk. There is limited evidence for the presence of viral RNA in breast milk, while there is neither evidence for active virus in breast milk nor transmission via breast milk. Currently, the primary concern is not whether the virus can be transmitted through breast milk, but rather whether an infected mother can transmit the virus through respiratory droplets. Precautions to avoid spreading the virus to the infant include the mother washing hands before holding her baby, and wearing a face mask when in close contact with her baby. Consult with your health care provider if you have questions or concerns.
Recent research has shown specific benefits of providing breast milk relevant to the COVID-19 situation. Researchers in China and in USA have recently found antibodies against the new coronavirus in the milk of mothers who had previously had COVID-19, further supporting the recommendation to continue breastfeeding.
—
Should mothers with COVID-19 be separated from their infants while infected with the virus and provide their babies expressed breast milk instead of feeding them directly at the breast?
The American Academy of Pediatrics (AAP) has issued a new guidance on July 22, 2020 regarding separation of mums and babies, based on the latest evidence. It is possible for mothers with suspected or confirmed COVID-19 to room-in with their newborns when precautions are taken to protect the infants from maternal infectious respiratory secretions.
As stated by UNICEF, the Academy of Breastfeeding Medicine, WHO and the CDC, if the mother and baby are able to remain together, breastfeeding at the breast is encouraged. Currently, the primary concern is not whether the virus can be transmitted through breast milk, but rather whether an infected mother can transmit the virus through respiratory droplets. Therefore, the CDC recommends the mother wear a mask and use good hand hygiene before and after breastfeeding.
—
Is breastfeeding safe considering the risk that I could get COVID-19? Should I switch to formula?
UNICEF states that breastfeeding is the safest, most reliable method of infant feeding in an emergency. An article in the Harvard Medical School Trends in Medicine mentions that given the risk that COVID-19 can spread through formula manufacturer factories and delivery warehouses, there is a risk of supply chain interruption if these factories and warehouses need to shut down.
Recent research has shown specific benefits of providing breast milk relevant to the COVID-19 situation. Researchers in China and in USA have recently found antibodies against the new coronavirus in the milk of mothers who had previously had COVID-19, further supporting the recommendation to continue breastfeeding.
Considering the benefits of breastfeeding and the current evidence of the insignificant role of breast milk in the transmission of other respiratory viruses, as stated by UNICEF, the Academy of Breastfeeding Medicine, WHO and the CDC, you can continue breastfeeding.
—
If I have COVID-19 and am too unwell to breastfeed or have been separated from my baby for a period of time, can I restart breastfeeding?
If you have been separated from your baby for a period of time and breastfeeding has been interrupted, re-establishing lactation when you are together with your baby again is generally possible and worth trying even if a return to full breastfeeding is not always achievable. The UNICEF UK guidelines can help you to re-establish your milk supply and continue breastfeeding. This is called re-lactation.
The WHO and UNICEF UK recommend the following essential measures for management of breastfeeding for re-lactation:
- Start actions to increase hormonal response, including plenty of skin-to-skin contact, nuzzling at the breast and breast massage.
- Breast massage and hand/pump expression (8-10 times in 24 hours) may help when separated from baby or in-between feeds
- The baby should suckle frequently from both breasts at least 8-12 times in 24 hours, at least 15 minutes on each breast. Consider night feeds.
- Try having the baby also at the breast while pumping.
- The baby should be well attached to the breast for effective suckling and to avoid nipple trauma.
- Monitor baby’s stool and urine output
- Contact an Infant Feeding Specialist to receive additional guidance and support to re-establish your milk production and control your baby’s growth.
—
Using breast pumps and other products
What are the storage guidelines for breast milk if I have COVID-19?
The Academy of Breastfeeding Medicine, WHO and the CDC state that although it is still unknown whether mothers with COVID-19 can transmit the virus via breast milk, limited studies on breastfeeding women with COVID-19 and other coronavirus infections have not detected the virus in breast milk. From that perspective, you can follow the regular breast milk storage guidelines (ABM and HMBANA).
If you have expressed breast milk cleanly and safely, you can store it at room temperature, in the fridge, or in the freezer, depending on how soon you want to use it.
| Storage place | Room temperature 16 °C to 25 °C (60 °F to 77 °F) | Refrigerator 4 °C (39 °F) or colder | Freezer -18 °C (0 °F ) or colder | Previously frozen breast milk thawed in the refrigerator |
| Safe storage time | Up to four hours is best Up to six hours for milk expressed under very clean conditions* | Up to three days is best Up to five days for milk expressed under very clean conditions* | Up to six months is best Up to nine months for milk expressed under very clean conditions* | Up to two hours at room temperature Up to 24 hours in the refrigerator Do not refreeze |
* Very clean conditions means rigorously following the guidance in our article on cleaning and sanitising your breast pump and those of the CDC. These guidelines for storing and defrosting breast milk are a recommendation – contact your lactation consultant or breastfeeding specialist for further information.
If your baby is in a neonatal intensive care unit (NICU) or special care ward, your hospital may have stricter recommendations for cleaning and storage.
If you’re refrigerating or freezing expressed milk, always label the bottles or bags with the amount and the date it was pumped, so you can track and manage your stored milk.
—
Could I get COVID-19 from a contaminated rental pump?
Trained employees perform the cleaning and servicing of rental pumps. The pumps are cleaned with water and soap and then disinfected before they can be used by another mother. There are many disinfectants, including commonly used hospital disinfectants, that are active against enveloped viruses, like the new coronavirus. Currently WHO recommendations include the use of:
- 70% ethanol to disinfect reusable dedicated equipment (e.g., thermometers) between uses
- Sodium hypochlorite at 0.5% (equivalent 5000ppm) for disinfection of frequently touched surfaces in homes or healthcare facilities
Alcohol-based disinfectants are approved for Symphony and have proven effective against SARS-CoV-2.
When using a breast pump to express breast milk, whether it is a rental pump or a store bought personal use pump, wash your hands before touching any pump or bottle parts and follow the CDC recommendations for proper pump kit cleaning after each use.
When it is time to return the Symphony pump to the rental station, please kindly disinfect the pump and the case.
—
What is the recommendation for use of Medela equipment if a mother is hospitalised due to Coronavirus disease?
According to the Academy of Breastfeeding Medicine, mothers who intend to breastfeed / continue breastfeeding should be encouraged to express their breast milk to initiate and build / maintain milk supply. If possible, a dedicated breast pump should be provided by the hospital. Prior to expressing breast milk, before touching any pump or bottle parts, mothers should wash their hands appropriately and take the necessary precautions such as wearing a face mask for at least 5-7 days until cough and respiratory secretions are dramatically improved. After each pumping session, all parts that come into contact with breast milk should be thoroughly washed following recommendations for proper pump kit cleaning and the exterior of the entire pump as well as the milk collection bottles should be properly disinfected using 70% ethanol or another disinfectant that is active against SARS-CoV-2.
—
How long is Coronavirus stable on surfaces such as pumps/kits/accessories?
Scientists have found that the virus responsible for COVID-19 was detectable as follow
in aerosols | for up to three hours |
on copper | up to four hours |
on cardboard | up to 24 hours |
on plastic | up to two to three days |
on stainless steel | up to two to three days |
How should I clean my pumping equipment if I have COVID-19?
When using a breast pump to express breast milk, wash your hands before touching any pump or bottle parts and follow the CDC recommendations for proper pump kit cleaning after each use. Recommendations encourage that someone who is not sick feed the expressed breast milk to the infant.
Does a dishwasher destroy the virus on milk collection sets for expressing mums?
While we still do not know much about this new coronavirus, SARS-CoV-2, most other viruses are believed to be deactivated at boiling temperatures. When using a breast pump to express breast milk, wash your hands before touching any pump or bottle parts and follow theCDC recommendations for proper pump kit cleaningafter each use.
For extra germ removal, sanitise pump parts at least once daily after they have been cleaned. Items can be sanitised using steam, boiling water, or a dishwasher with a sanitise setting.
—
Does boiling pump accessories in water kill coronavirus?
While we still do not know much about COVID-19, most other viruses are believed to be deactivated at boiling temperatures. When using a breast pump to express breast milk, wash your hands before touching any pump or bottle parts and follow the CDC recommendations for proper pump kit cleaning after each use.
For extra germ removal, sanitise pump parts, wash basin, and bottle brush at least once daily after they have been cleaned. Items can be sanitised using steam, boiling water, or a dishwasher with a sanitise setting.
—
Is dry air storage of pumping accessories between expressions safe?
Yes. After each pumping session, all parts that come into contact with breast milk should be thoroughly washed following CDC recommendations for proper pump kit cleaning which state that clean pump parts, bottle brushes and wash basins should be allowed to air-dry thoroughly before storing to help prevent germs and mould from growing. Once completely dry, the items should be stored in a clean, protected area to prevent contamination during storage.
—
The Calma bottle/ nipple shields /feeding devices / pacifiers are to be washed after use. Can they be sanitised more frequently?
Infant feeding devices, bottles, teats and pacifiers should be cleaned after use following the CDC cleaning recommendations for infant feeding items.
For extra germ removal, at least once daily after the items have been cleaned, items should be sanitised using steam, boiling water, or a dishwasher with a sanitise setting.
If your baby is hospitalised, follow your health care provider’s instructions for cleaning infant feeding items.
—
General
How can I protect myself and others?
Official bodies like WHO and UNICEF recommend
- washing our hands frequently and thoroughly with water and soap or sanitiser and avoiding close contact with people who are ill. Furthermore, not touching your eyes, nose and mouth with unwashed hands
- catching coughs and sneezes in a tissue, binning it in a sealed waste bin and washing your hands as all this helps minimise the risk of infection and disease spreading.
- avoid shaking hands, hugging or kissing people while greeting.
- avoiding close contact with people who are obviously ill.
- social distancing (keep enough distance to other people).
- stay home if you feel unwell. If you have a fever, cough and difficulty breathing, seek medical attention and call in advance. Follow the directions of your local health authority.
—
How do I protect my baby against COVID-19?
Breast milk is the best source of nutrition for most infants, and provides protection against many illnesses. But, as the CDC notes, there is much unknown about this virus. If you are pregnant or breastfeeding, we recommend that you look at the CDC’s guidance and connect with your healthcare provider if you have any specific concerns.
- Clean hands often using soap and water or alcohol-based hand sanitiser
- Avoid people who are sick (coughing and sneezing)
- Clean and disinfect high-touch surfaces daily in household common areas (e.g. tables, hard-backed chairs, doorknobs, light switches, remotes, handles, desks, toilets, sinks)
- Launder items including washable plush toys as appropriate in accordance with the manufacturer’s instructions. If possible, launder items using the warmest appropriate water setting for the items and dry items completely. Dirty laundry from an ill person can be washed with other people’s items.
A complete review of the CDC guidelines regarding COVID-19 can be found at: www.cdc.gov/coronavirus/2019-ncov/specific-groups/pregnancy-guidance-breastfeeding.html.
In addition, UNICEF’s recommendations can be found at:
www.unicef.org/stories/novel-coronavirus-outbreak-what-parents-should-know
Consult with your health care provider if you have further questions or concerns.
—
How does Coronavirus (COVID-19) spread?
Much is still unknown about how the disease is spread. UNICEF and WHO state that person-to-person spread occurs mainly by breathing in respiratory droplets produced when an infected person coughs or sneezes, similar to how influenza (flu) and other respiratory pathogens spread. These respiratory droplets also land on objects or surfaces and people touching surfaces contaminated with the virus can get infected by touching their eyes, nose or mouth with their contaminated hands. The COVID-19 virus may survive on surfaces for several hours, but simple disinfectants can kill it.
—
What are the symptoms of a coronavirus infection?
The main symptoms include
- fever (>37.8 degrees Celsius / >100.0 degrees Fahrenheit),
- cough, i.e. acute (newly developed) cough and/or
- shortness of breath or breathing difficulties and/or tiredness
—
Disclaimer
The information and materials provided on this website does not, and is not intended to, constitute legal advice; instead, all information available on this site are for general informational purposes only. Information on this website may not constitute the most up-to-date information. Medela reserves the right to supplement this website at any time or to change or delete any information or materials on this website.
This website contains links to other third-party websites. Such links are only for the convenience of the reader, user or browser; Medela does not recommend or endorse the contents of the third-party sites.
The information and materials on this web site is provided “as is”; no representations are made that the content is error-free. Whilst we have tried to ensure the accuracy and completeness of the information and materials on this website, we do not warrant or guarantee the accurateness, completeness, adequacy or currency of the information and materials contained in or linked to this website.
All liability with respect to actions taken or not taken based on the content of this website are hereby expressly disclaimed. Your use of content contained in or linked to this website is entirely at your own risk. Medela accepts no liability for any loss or damage howsoever arising out of the use of this website or reliance on the content of this website.
Last update: 5 August 2020